CLIENT SUCCESS
$17 Million Proof That Payer-Provider Partnership Solves the Patient Billing Problem
Allegheny Health Network and Highmark worked together to reduce patient billing and insurance friction and deliver a uniquely integrated financial experience.
The Challenge
For Allegheny Health Network and Highmark, the goal isn’t just better healthcare, it’s better health. But too often, patient billing and insurance friction stood in their way. While Allegheny Health Network had taken meaningful steps to simplify their billing process, patients could still get overwhelmed by the disconnected bills and explanations of benefits (EOBs) piling up in their mailboxes. Not only did it compound stress patients already had about their health, but it also led to missed payments and costly customer service inquiries.
It was clear that providers alone are unable to address the structural challenges of confusing bills, uncoordinated EOBs and fragmented communications. To truly fix the patient billing problem, Allegheny Health Network and Highmark partnered with Cedar to create a single source of truth across the provider and payer.
The Solution
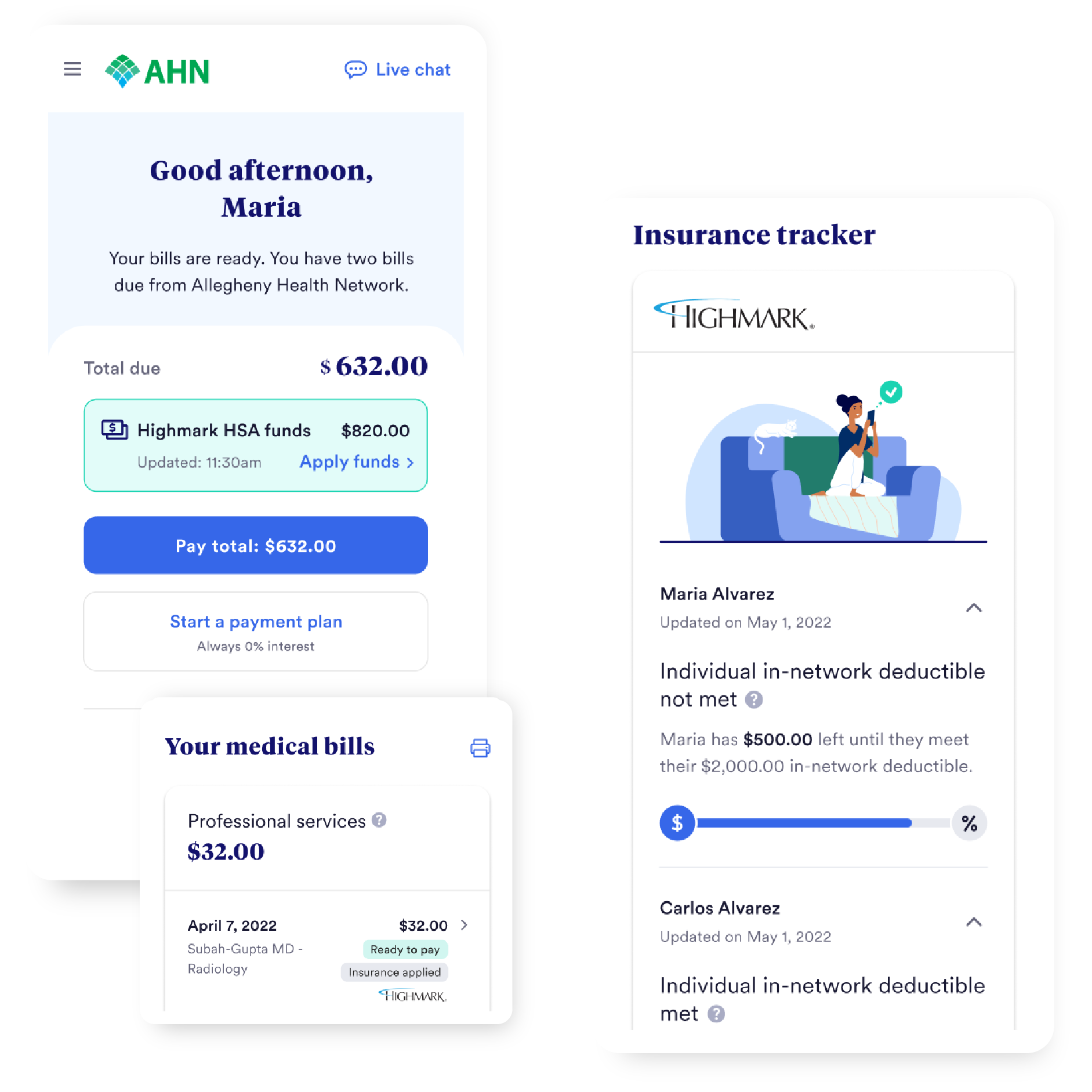
In October 2022, Allegheny Health Network and Highmark radically simplified their customer financial experience by launching Cedar Pay, which included a new set of capabilities powered by Cedar’s Payer Intelligence Layer. With the Payer Intelligence Layer, Allegheny Health Network uniquely incorporates Highmark into patient bills, providing a streamlined path to resolution.
In less than one year with Cedar Pay, Allegheny Health Network added $17 million in patient payments, thanks in part to the integration with Highmark.1 But the clearest signal that payer-provider partnership was working came from patients themselves, who gave the integrated experience a 90% satisfaction rating.2
“Cedar has shown us that if you make it easy, if you deliver transparency, and if you provide the right information when people need it the most, you can create a remarkable health experience that frees people to be their best.”Vice President of Customer and Clinician Experience Solutions, Highmark
“I’ve been impressed by how much Cedar’s payer integration affects patient engagement. I have my provider saying this is good to go. I have my insurance saying it’s good to go. Great, I can pay with confidence."Director of Revenue Cycle Strategic Initiatives and Optimization, Allegheny Health Network
Highmark Health’s primary goal is for customers to feel happy, satisfied, and confident in the information they’re receiving. We want them to return to Allegheny Health Network or continue their coverage with Highmark because we work together to make it so simple and easy."Vice President of Customer and Clinician Experience Solutions, Highmark
- Based on the comparison between pre-Cedar (October 2021-September 2022) and post-Cedar (October 2022-July 2023) Allegheny Health Network patient billing and payment data
- Based on the available Cedar-serviced patient data for Highmark members at Allegheny Health Network as of May 2023 (Total number of patients: 5,563; start of time period: 11/1/2022; end of time period: 05/17/2023)